Connect With Us
Wound Care

Wound care is particularly important for those with diabetes. It’s possible that what appears to be a small wound could turn into more severe foot complications down the road if left untreated. It’s common for those with diabetes to experience neuropathy. Neuropathy is a type of nerve damage that affects the body and can cause you to lose feeling in the feet. If you’re no longer experiencing feeling in your feet and a wound develops, it’s very possible it may go unnoticed if you don’t check your feet daily.
Some factors that contribute to the formation of wounds on the feet include wearing tightly fitted shoes, getting a pebble stuck in your shoe, or simply walking. What may appear to be just a small inconvenience such as a blister or callus can worsen over time, so it’s important to be safe and seek the attention of a professional. If you’ve developed a wound, it’s recommended that you try your best to keep the weight off of the area until you’re able to meet with a podiatrist.
Some ways to prevent wounds from developing include checking your feet daily for any injuries, washing and drying your feet daily, dressing for comfort and making sure your toes have enough space, and properly trimming your toenails straight across. Because wounds can lead to more severe complications, especially for those with diabetes, we recommend you speak with a podiatrist for professional guidance and a suggested plan for treatment.
Diabetic Foot Ulcers (DFUs)
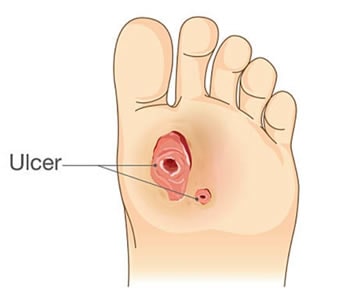 These are wounds that often occur on the bottom aspect of foot, on top of toes or on the heel. Diabetic foot ulcers usually start as a thickened callus that develops with walking. Over time, the skin breaks down, leading to open sore formation.
These are wounds that often occur on the bottom aspect of foot, on top of toes or on the heel. Diabetic foot ulcers usually start as a thickened callus that develops with walking. Over time, the skin breaks down, leading to open sore formation.
Risk Factors for developing diabetic foot ulcers include:
- Diabetes
- Lack of sensation
- Foot deformity
- Arterial disease
- Obesity
- Smoking history
- Poor Nutrition
- Immobility
Venous Leg Ulcers (VLUs)
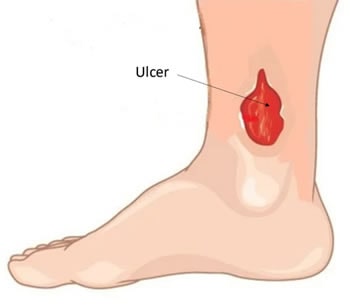 Venous leg ulcers are open sores that usually occur on the inside of the ankle region of the lower leg. VLUs seldom occur above the knee and are not typically seen on the foot or toes. These wounds can be painful and heavily draining. Often patients will also have a history of leg swelling, varicose veins or blood clots of the leg.
Venous leg ulcers are open sores that usually occur on the inside of the ankle region of the lower leg. VLUs seldom occur above the knee and are not typically seen on the foot or toes. These wounds can be painful and heavily draining. Often patients will also have a history of leg swelling, varicose veins or blood clots of the leg.
Risk Factors for developing venous leg ulcers include:
- Obesity
- High blood pressure
- Heart failure
- Previous leg surgeries
- Blood clots of the leg
- Kidney disease
- Female gender
- Pregnancy
- Long hours standing
- Immobility
